Healthcare automation
works for you, so you can focus on them
Streamline your Healthcare Operations for greater efficiency so you can focus on patients and create a centralized Community of Care.

Medicare Prior Authorization Made Easy with AI and RPA Medical Solutions
At qBotica, we can help you harness the power of Robotic Process Automation in healthcare and intelligent document processing (IDP) to streamline your business processes and improve your efficiency. Whether you need to automate your Medicare prior authorization requests, extract data from complex documents, or integrate them with your existing systems, we have just the right solution for you.
Our healthcare RPA solutions can be customized to fit different providers’ and specialists’ specific needs and workflows. Here’s how.
Forrester
225,000
Hours saved by automation after three years.
McKinsey
$1 trillion
Known improvement opportunities in healthcare.
Accenture
30 – 40%
Lower cost of underwriting and claims processing with automation.
Streamlined Healthcare Automation Solutions
Amidst a sea of specialized Healthcare solutions, the qBotica Healthcare Automation Platform encompasses every aspect.

Lower cost of care
Promote seamless collaboration between payers and providers to reduce expenses.

Data-driven healthcare
Revolutionize healthcare processes from relying on documents to adopting intelligent, data-driven processes.

Wholistic view of data
Consolidate all essential information and valuable insights in a centralized location to enhance decision-making efficiency.

Empowered workforce
Streamline processes to enhance staff retention, bolster their experience, and facilitate upskilling by minimizing manual work.
The Complex World of Medicare Prior Authorizations
That’s where qBotica comes in.
qBotica is one of the leading providers of robotic process automations in healthcare revenue cycle management companies. qBotica’s RPA in healthcare can help providers automate and streamline their Medicare prior authorization processes, reducing errors, delays, and denials.qBotica’s RPA in healthcare solutions can:
- Monitor and update Medicare prior authorization rules and requirements in real-time
- Identify and flag services or items that require automated prior authorization
- Extract and validate relevant data from electronic health records (EHRs) and other sources
- Generate and submit prior authorization requests electronically or via fax
- Track and follow up on the status of prior authorization requests
- Notify providers and patients of prior authorization decisions
- Appeal denied or partially approved automated prior authorization requests
- Integrate with billing and claims systems to ensure accurate and timely payment
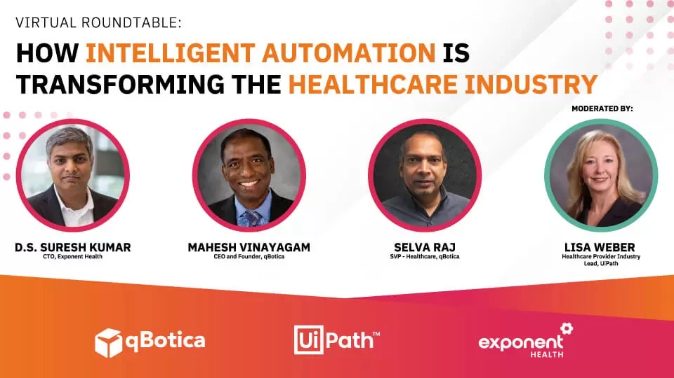
Watch our Latest Webinar
RPA for Healthcare Transformation
Watch the qBotica Virtual Roundtable event to discover how cutting-edge technologies such as AI, RPA, and Automation as a Service are revolutionizing the healthcare landscape by minimizing administrative tasks and optimizing work processes.

Transforming Specialty Healthcare: Leveraging AI for Superior Delivery
Join us in this exclusive webinar that will explore the transformative power of AI and automation in the healthcare industry, particularly for specialty providers.
Revolutionizing the Healthcare Industry
qBotica has demonstrated its leadership and innovation in the healthcare industry through its revenue management solutions healthcare. We offer various revenue cycle management services that help healthcare providers improve their financial performance and patient satisfaction.
Medical revenue cycle management
Denial management in healthcare
Patient access services
Coding and billing services
And much more!
We have helped several revenue cycle management healthcare companies significantly improve their key performance indicators, such as days in accounts receivable, denial rate, or even net revenue.
Partnering for Success: qBotica’s Collaborations and Client Achievements
qBotica is a leading provider of intelligent automation in the healthcare industry. We help businesses optimize their processes and enhance their customer experience.
qBotica has partnered with some of the most prestigious organizations in various industries, such as Microsoft, the University of Phoenix, Western Union, and many more. These collaborations have resulted in successful outcomes and recognition for both qBotica and its clients.
Thanks to us, companies have been able to:

Process more than 50 million documents.

Automate their processes and alleviate the workload for their employees.

Gain a competitive advantage in their respective industries
qBotica’s most notable partnership is its collaboration with UiPath, the global medical RPA leader.
qBotica and UiPath have jointly developed the automation cube, a comprehensive framework that enables enterprises to design, implement and manage RPA projects effectively. The automation cube covers all aspects of RPA medical, including:
Strategy
Governance
Development
Maintenance
It also leverages qBotica’s expertise in artificial intelligence, machine learning, natural language processing, and computer vision to enhance the capabilities of UiPath’s platform. As a result of this collaboration, qBotica has achieved platinum-level partnership status with UiPath, the highest level of recognition for UiPath partners.
Top Automation Areas
Top Areas of Automation for Healthcare Providers & Payers

Healthcare providers
Patients and paperwork shouldn't be at odds when it comes to receiving care.
Buried beneath the piles of healthcare claims processing documents on a provider’s desk and lost amidst the influx of emails in their inbox lie stories waiting to unfold: A patient grappling with a health challenge in dire need of resolution.
qBotica utilizes cutting-edge technology and industry best practices to identify bottlenecks, reduce denials, and maximize revenue for our clients.
Patient Access
Accelerate the patient care process efficiently.
The journey of patient care commences well in advance of their actual visit to a healthcare provider. By leveraging Healthcare automation, we can expedite the essential pre-work involved in onboarding patients, such as insurance verification, data collection, scheduling, and more. This approach not only ensures that individuals in need of care swiftly become patients but also enhances the revenue cycle management (RCM) process.
Ask us about these business use cases:
- Patient Onboarding
- Scheduling
- Insurance Verification & Eligibility
- Document Intake
- Referrals Management
- Point-of-Service Collections
- Financial Clearance & Planning Initiation
- Appointment Reminders
- Outreach
- Pre-Certification & Prior Authorization Submissions
Care Delivery
Customize care to expedite the healing process.
Collecting, arranging, and comprehending patient data should not hinder healthcare providers from delivering individualized care. By implementing Healthcare automation in healthcare, providers can create tailored care plans and get the healing process back on the right path.”
Ask us about these business use cases:
- Charge Capture & Coding
- Documentation
- Lab & Radiology Reports Triaging
- Check-In
- Check-Out
- Lab Order Entry Collections
- Dx, X-Ray, & Radiology Order Entry
- Medication Management
- Phone Triage & Follow-Up Calls
- Remote Visits & Monitoring
Revenue Cycle Management
Accelerate your revenue generation.
Streamlining outdated claims processes, simplifying patient payment plans, and reducing time-consuming audits are obstacles that hinder providers from achieving timely revenue realization.
By embracing healthcare automation in revenue cycle management healthcare, you will gain access to the necessary resources to deliver effective and innovative care programs and services. This, in turn, will enable you to attract and retain top medical professionals.
Ask us about these business use cases:
- Automated Prior Authorization
- Healthcare Claims Processing – Posting
- Patient Payment – Posting
- Coordination of Benefits: Primary, Secondary, & Tertiary
- Price Transparency & Real-Time Estimates
- Revenue Integrity – Payment Audits (Under & Over)
- Provider: Insurance Enrollment
- Revenue Integrity – Charge Description Master (CDM) Management
- Revenue Integrity – IME or IMR Audits (CMS & Medicare Advantage)
- Insurance Claims – Denied & Rejected Follow-Up
Practice Management
Streamline Processes. Enhance Care Quality.
You can identify the signs of administrative friction when healthcare providers spend more time clicking on a computer mouse instead of engaging with patients, and the staff is unable to handle the necessary tasks that ensure the smooth and safe functioning of healthcare organizations.
Ask us about these business use cases:
- Clinic Staffing & Scheduling
- Regulatory & Compliance Reporting
- P&L Reporting
- Charge Capture, Documentation & Coding Audits
- HEDIS Reporting
- Indexing & Routing Documentation
- Care Coordination
- Patient Communications
- Population Health Management
- Disease Tracking & Trending
Healthcare Payers
You are not just an insurance payer; you are a Healthcare partner.
Payer organizations play a vital role in the healthcare industry by handling crucial health insurance payment processes. However, forward-thinking individuals recognize that they have the potential to make a more significant impact in the realm of member and provider healthcare. By leveraging qBotica’s Healthcare automation, you can not only enhance the efficiency of traditional payer processes but also establish yourself as a unique and valuable healthcare partner for both providers and members.

Claims Management
Simplify & modernize Healthcare claims processing.
Transforming claims decisions doesn’t require a labor-intensive approach that comes with a hefty administrative cost. The integration of intelligent Healthcare automation provides you with the ability to minimize errors while effortlessly streamlining adjudication processes.
Ask us about these business use cases:
- Multi-Channel Intake
- Member & Provider Info Edits
- Member Eligibility Validations
- Medical Necessity Validations
- Review Case Determination
- Claim Processing Audit
- Claims Adjudication
- Claim Payment Adjustments
- High Dollar Claims Audits
- Post-Authorization Case Review
Care Management and Behavioral Health
Transforming care programs into personalized experiences.
As an essential healthcare collaborator, our aim is to provide groundbreaking initiatives that enhance clinical results and guarantee timely treatment for vulnerable individuals. With a comprehensive understanding of patient health data and personalized member insights, we can effectively collaborate with healthcare providers and engage with members to achieve optimal outcomes.
Ask us about these business use cases:
- High Risk Member Identification
- Member Outreach Scheduling
- Risk Assessment
- Personalized Care Plan
- Duplicate Case Identification & Merge
- Eligibility Management
- Questionnaire Management
- Member Clinical History Data Gathering
- Member Correspondence Letter Generation
- Scheduling Appointments
- Monitoring Progress
Provider Management
Effortlessly streamlines and utilizes provider data.
When the task of managing healthcare data becomes excessively time-consuming and labor-intensive, it becomes almost impossible to utilize that data effectively to enhance the experiences of both healthcare providers and patients. The Implementation of Healthcare automation for managing provider data empowers payers to play a central role in assisting providers in reducing costs and helping patients achieve their health objectives. Ask us about these business use cases:- Provider Request Document Checklist
- Roster Data Formatting & Mapping
- Update Provider Data
- Provider Data Correction – NPI, PHIN, PIN
- Provider Correspondence & Notifications
- Sanctions Validation
- Provider Taxonomy Management
- NPI, Education & Address Validation & Verification
- Provider Contract Setup
- Payment Reconciliation
Contact Center
Excellence in Every Interaction: Achieving a Perfect Score
The importance of your Net Promoter Scores (NPSs) cannot be understated. It is vital for your call center to deliver precise information when addressing inquiries to maintain a favorable reputation with both providers and members.
Ask us about these business use cases:
- Account Inquiries & Benefit Look-Up
- Claims Status Request
- Insurance Verification
- Plan 360 View & Care Coordination
- Pre-Certification & Authorization Status Check
- Previous Call History Summary
- Address Validation & Changes
- Member Demographics Updates
- COB Inquiries
- Claim Billing Inquiry
More To Explore in Automation for Healthcare
Don’t miss these resources, upcoming events, and recaps
How qBotica can Help You
qBotica is a leading provider of claim processing system in healthcare, using advanced artificial intelligence and automation to streamline your workflows and reduce errors. Our robotic process automation for healthcare can help your prior authorization company save time and money, improve patient satisfaction, and comply with regulatory standards.
qBotica also offers healthcare revenue cycle management services tailored to your needs and goals. Whether you need to optimize your billing, coding, collections, or denials management, qBotica has healthcare revenue cycle management solutions for you. qBotica can help you increase your revenue, reduce costs, and enhance your cash flow. Take advantage of this opportunity to transform your healthcare business with qBotica.
Contact us today to schedule a free consultation and demo of our services.
Latest Case Studies and Customer Success Stories
FREQUENTLY ASKED QUESTIONS
Revenue cycle management or RCM in healthcare refers to the process of managing the financial transactions and interactions between healthcare providers and patients throughout the entire care continuum, from patient registration and appointment scheduling to claims submission, payment collection, and revenue reconciliation.
Yes. A revenue cycle management system can reduce claim denials by
- implementing proactive denial prevention strategies
- conducting regular audits to identify root causes of denials
- improving coding accuracy
- streamlining documentation processes
- leveraging technology for claims scrubbing and validation
At qBotica, our revenue cycle management -
- leads to improved cash flow
- reduced accounts receivable days
- increased revenue capture
- enhanced billing accuracy
- lower administrative costs
- greater transparency into financial performance metrics.
Our revenue cycle management solutions enhance the patient experience by
- Reducing wait times
- Providing accurate cost estimates
- Offering convenient payment options
- Resolving billing inquiries promptly
- Better transparency in financial transactions